Perks of Being a Private Practice Doctor
Private Practice Doctor vs. HMO Employee
If you were to ask a physician about the biggest decision they had to make in their medical journey, they’d probably say deciding on their specialty. This choice will weigh heavily on their future happiness and work/life balance. Their second most significant decision, though, would be whether they opt for a private practice setting or employment with a large hospital network or corporation. It is equally important, although the decision comes at a later point in their career so there is more time to consider.
In the past ten years, there has been a pretty big shift between the two and now, less than half of physicians are working in private practice. More and more are opting for working in hospitals as direct employees. Despite these numbers, private practice is still on the radar and should be.
The idea of opening a private practice for many is a dream, and rightfully so since you can be your own boss and that is the goal of many. It’s important to keep things in perspective though and consider all the benefits and drawbacks and how they compare to working in a big hospital. We lay them out here and share insight from two recently retired physicians, both who opted for private practice.
Benefits of Private Practice for Doctors:
1. Enhanced Autonomy
Private practice doctors relish the freedom to steer their professional journey. Unlike their counterparts in institutional settings, these doctors dictate their schedules, treatment modalities, and the overall direction of their practice. This autonomy fosters a sense of professional fulfillment, empowering doctors to cater to patient needs with unparalleled flexibility. If they wanted to put a new sign outside their practice, they could do so without going through any red tape. The bigger the healthcare network you work for, if you choose that route, the less autonomy you would.
“Decisions can be made and acted on quickly. You set the tone and focus of your practice. If something comes up and you need to adjust your schedule, you just do it. If you decided you’d rather work an hour later each day and see fewer patients per hour, you just do it. You are much more aware of how everyone else is doing at their job from custodial workers to other providers because it all affects you directly,” says retired family medicine specialist, Dr. Guyton Winker.
2. Meaningful Patient Relationships

The heart of private practice lies in the profound relationships doctors build with their patients. With ample time for comprehensive consultations, private practice doctors delve deep into patient concerns, crafting personalized treatment plans that prioritize individual needs. Many private practice doctors know patients by name and may even know family members by name. This patient-centric approach not only elevates the quality of care but also fosters trust and loyalty, driving superior patient outcomes. There are also less guidelines you have to adhere to (ex: meeting a quote of patients seen per day), so the interactions are more likely to be hyper intentional. The patients being seen by a doctor in private practice are less likely to be a number.
3. Job Security
In the ever-evolving landscape of healthcare, job security is a prized asset. Private practice doctors enjoy a semblance of stability, shielded from the uncertainties of institutional restructuring and layoffs. By cultivating a loyal patient base and nurturing referral networks, these doctors fortify their practice against external market forces, ensuring a steady stream of patients and income.
“The security in this situation is that you know you aren’t going to make decisions you don’t like, as you are part of the decision-making,” says retired orthopedic surgeon, Dr. Kim Chillag, who was in private practice for over twenty years.
4. Cultivating Ideal Work Culture
Private practice empowers doctors to shape their ideal work culture. Whether fostering a collaborative environment among staff, embracing cutting-edge techno00logies, or prioritizing work-life balance, doctors curate a practice ethos that resonates with their values. This autonomy not only enhances job satisfaction but also attracts like-minded professionals, fostering a culture of excellence and patient-centric care.
5. Potential for Higher Earnings
Earnings beckon doctors, whether in private practice or not. It’s a lot of what doctors determine success by. By setting competitive fee schedules, diversifying services, and optimizing practice efficiency, private practice doctors unlock the potential for higher earnings, emphasis on potential.
“Your earnings depend on how valuable you are as a physician. If you are an esteemed physician and good at what you do, you can make money anywhere,” says Dr. Chillag.
A recent 2023 study by Medscape shows that self-employed physicians reported earning $374,000 on average while those employed by a network or corporation earn on average $344,000. There seems to be a slightly bigger advantage to working in private practice when it comes to earnings. And while this is the average across all specialties, some individual specialties can earn up to a million if they are especially entrepreneurial.
6. Fulfilling Entrepreneurial Journey
Private practice embodies the spirit of entrepreneurship, offering doctors a platform to realize their business aspirations. From establishing a distinct brand identity to devising innovative marketing strategies, private practice doctors navigate the complexities of business ownership with zeal. This entrepreneurial journey not only fosters personal and professional growth but also instills a sense of pride in the practice's achievements.
“If you are truly inspired to do the extra work, and crave independence, private practice would be for you,” says Dr. Winker, “but keep in mind practice ownership is another full-time job.”
Drawbacks of Private Practice for Doctors:
1. Potential Financial Risk
Despite the allure of higher earnings, private practice entails financial risks. From managing overhead costs to navigating reimbursement complexities, doctors grapple with financial uncertainties that can impact practice viability. Economic downturns or regulatory changes further compound these challenges, necessitating vigilant financial management to safeguard practice stability.
“You have no guaranteed income. If something like a worldwide pandemic comes along, and your patient volume tanks, so does your income,” says Dr. Winker.
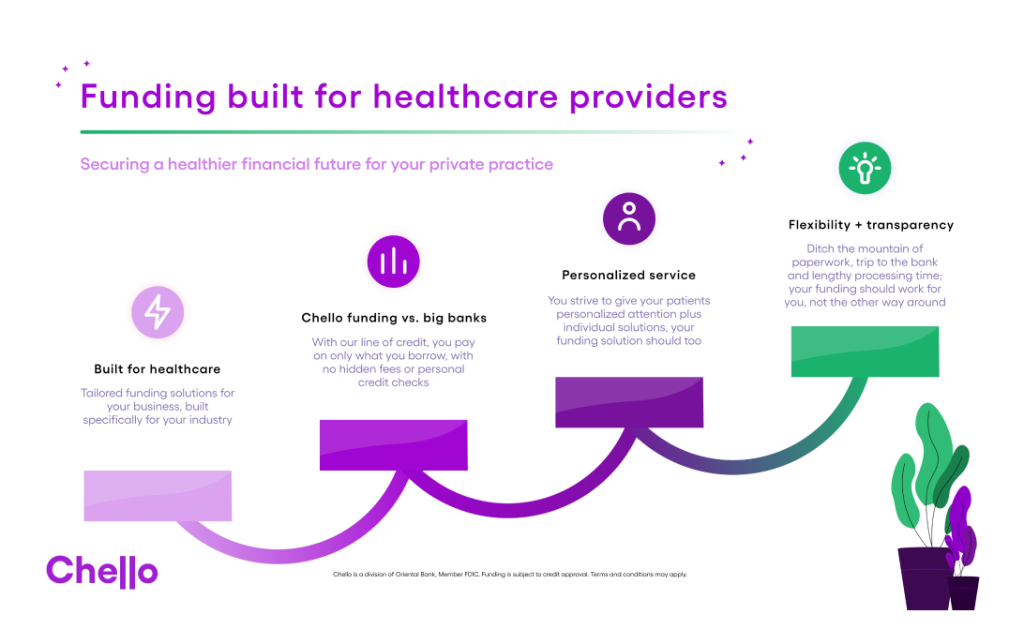
This is where new technology tools in the industry that help predict cash flow, like Chello, can be super useful. They help take the guesswork out of where your practice will be in nine days or 90 days. They help to ensure your financials are more secure and that you have a plan in plan if anything unexpected were to happen.
2. Administrative Burden
The administrative demands of private practice weigh heavily on doctors. From billing and coding to regulatory compliance and documentation, doctors devote significant time and resources to administrative tasks, detracting from patient care. While outsourcing administrative functions or leveraging practice management software can alleviate some burdens, doctors must strike a delicate balance between efficiency and clinical excellence.
“If you worked for a large network, you are an employee. You show up for work. You don’t have to worry about hiring another x-ray tech or payroll,” says Dr. Chillag.
If you feel like the administrative burden of being a private practice doctor may be too much, there are certainly ways around it. You have the option of hiring an experienced office manager or financial executive to handle all of the business aspects of the practice so that nothing of the sort weighs on your mind.
3. Limited Resources and Infrastructure
Unlike large healthcare institutions, private practices often operate with limited resources and infrastructure. Outdated technology, understaffing, and constrained marketing budgets pose formidable challenges for private practice doctors. Investing in practice enhancements or expanding services may require substantial upfront capital, further stretching resource allocation.
It's best practice for small to medium sized healthcare practices to establish a line of credit, that way if any big hiccups where to occur in financing, they’ll have a fail-safe in place. Their resources can easily go form limited to not.
4. Professional Isolation
Despite autonomy, private practice doctors may experience professional isolation. Solo practitioners or small group practices lack the peer support and collaborative opportunities inherent in institutional settings. This isolation impedes professional growth and hampers doctors' ability to stay abreast of industry advancements.
Again, there are ways around this. You could join mastermind or consultation groups within the area or attend conferences and networks to expand your social and professional network.
Private practice offers numerous advantages such as autonomy, flexibility, and potentially higher earning potential, allowing healthcare professionals to tailor their services to meet the unique needs of their patients. However, it also comes with its own set of challenges, including the financial risks, administrative burdens, and the need for effective marketing and business management skills. Ultimately, the decision to pursue private practice should be carefully considered, weighing the pros and cons against one's individual career goals, values, and personal circumstances.
While it may not be the right choice for everyone, for those willing to navigate its complexities, private practice can be a fulfilling and rewarding career path in the healthcare industry. A private practice setting, one owned solely by physicians, can be a very strong option for you are wanting to be your own boss and be in control of where you will land in the future.